Hepatitis C Blog
Greg Jefferys Hepatitis C blog deals with all the issues associated with hepatitis C
Is Liver Damage from Hep C Reversible
- February 23, 2021
- By Greg Jefferys
- 1 Comment
(This post is still under construction)
Hep C, Liver Damage and Liver Cirrhosis
Hepatitis C is one of the major causes of liver fibrosis and liver cirrhosis, which leads to death from liver failure. So one of the big questions that people who have had Hep C is: “Is liver damage from Hep C reversible?”
Put simply the answer is yes, liver damage from Hepatitis C can be reversed and the liver can heal from even advanced cirrhosis. The liver is very capable of regenerating from significant damage because, but various factors combined with a Hep C infection can reduce the liver’s ability to regenerate.
In this post, I will explain exactly what Hep C-induced liver cirrhosis is and give you an easy-to-understand explanation of what you can do to reverse liver damage caused by Hepatitis C once the Hep C infection is cured.
What is Liver Cirrhosis from Hep C?
Liver cirrhosis is caused by scar tissue forming in the liver due to damage caused by the Hep C virus, which “breeds” inside liver cells. As the amount of scar tissue increases it distorts the shape of the liver and can cause swelling and inflammation.
Liver cirrhosis is the leading cause of liver cancer (HCC).
As the amount of scar tissue (fibrosis) increases the ability of the liver to perform its function decreases until the liver can no longer function, resulting in liver failure and death.
Diagnosis of liver fibrosis
There are varieties of methods for making the diagnosis of liver fibrosis, which can be classified into invasive and non-invasive approaches.
Invasive approach – liver biopsy examination
For invasive approach, it refers to liver biopsy examination, which provides liver tissue for a histopathological assessment of liver. Liver biopsy examination can be done percutaneously, transvenously (either transjugularly or transfemorally), or surgically (open or laparoscopic operations).[6] Indications for liver biopsy are for diagnostic and/or prognostic purposes, as well as for treatment planning.[7]
Liver biopsy is still regarded as the gold standard for liver fibrosis assessment in various chronic liver diseases.[8,9] Apart from general histological staging, liver biopsy can also provide information concerning morphometry, which can provide additional information on the distribution and the exact quantity of liver fibrosis.[10] A recent quantitative tool called qFibrosis utilized 87 parameters aiming for combining the results of collagen patterns, collagen architectural features and statistical analysis of features of respective collagen patterns into a single index. This requires an unstained biopsy sample for the automated analysis of liver fibrosis staging.[11] All these evidences illustrate that liver biopsy plays an important role in the diagnosis of liver fibrosis.
Apart from liver fibrosis staging, liver biopsy can provide different information important for the management of the clinicians. For example, in cases of NAFLD, the degree of necroinflammation and steatosis can be determined by liver biopsy so corresponding management can be provided for this potentially reversible situation.[12] Liver biopsy is also helpful in diagnosing adverse drug reaction and classification of liver tumors.[13] Yet, the most common reason for conducting a liver biopsy is for assessing the liver fibrosis in patients with chronic viral hepatitis and NAFLD.
Such a direct and useful method bears quite a few limitations. Sampling error is a major limitation for liver biopsy as only 1/50,000 of the whole liver parenchyma is obtained. Sampling error can be minimized by either obtaining a specimen of sufficient size (at least 2 cm in length) or from different lobes, which may not be feasible all the time.[14] Well reported complications from liver biopsy examination include pain,[15] bleeding such as wound bleeding, intraperitoneal hemorrhage, hemobilia or hemothorax,[15] transient acute hypotension or vasovagal syncope.[16] Fatal complications like uncontrolled bleeding, bacteremia and sepsis are rare but still possible.[17] In patients with HCC, liver biopsy also carries a risk of spreading the cancer cells.[18]
Non-invasive approach
Radiological assessments are either ultrasonographic-based [e.g. transient elastography, acoustic radiation force impulse (ARFI) imaging and shear wave elastography (SWE)] or magnetic resonance (MR)-based [i.e. MR elastography (MRE)].
Ultrasonographic based
Transient elastography
Transient elastography (Fibroscan®, Echosens, Paris, France) assesses liver stiffness measurement (LSM) by transmitting shear wave followed by ultrasound wave through a probe putting on the skin overlying the liver parenchyma. The velocity of the shear wave passing through the liver parenchyma is calculated by Doppler technique. The higher the velocity, the stiffer the liver parenchyma is. As mentioned by the manufacturer, for an examination to be considered as reliable, it requires at least 10 successful attempts and the ratio of interquartile range to median of those measurements should be less than 0.3.[19] LSM reflects the degree of liver fibrosis.[20] It can even identify those with no or minimal fibrosis and differentiate them from those with severe fibrosis or cirrhosis.[21] It has been proved useful across different liver disease entity (e.g. chronic hepatitis B and C, autoimmune hepatitis).[22] However, LSM by transient elastography is found to be less reliable in obese patients.[23,24] It can be less accurate in certain situation, e.g. severe acute exacerbation of hepatitis,[25] post-treatment fibrosis stages in CHB[26] or chronic hepatitis C (CHC) patients.[27]
ARFI imaging
ARFI is another technique for estimating liver fibrosis. It is implemented in current ultrasound scanner, without acquirement of external equipment. The conventional ultrasound probe automatically produces an acoustic “push” pulse for generating shear-wave which passes through the tissue. The wave propagation speed is assessed. Again, higher the speed, higher the liver stiffness measurement is.[28,29] There are several advantages for ARFI. As it is a function of the ultrasound scanner, no additional cost is required.[30] The ARFI not only shows the degree of fibrosis, it also provides external information for disease progression for different chronic liver disease, for example HCV.[31] Another advantage of this tool is that it can provide real-time results and easy to perform. The measurement results appear to be more accurate in overweight and obese patients, compared with transient elastography.[32] However, one prominent disadvantage for ARFI is that the range of its measurement is quite narrow (only from 0.5 to 4.4 m/s).[33] Furthermore, it is quite difficult to match the degree of fibrosis with the wave propagation speed, i.e. a cut-off, which is difficult to be defined.[34]
SWE
SWE is a 2-dimensional ultrasound technique based on the estimation of shear wave velocity from the radiation force of a focused beam of ultrasound,[35] and it can be converted results in terms of kPa by an equation.[36] No extra vibrator or detector is required as it is integrated into a conventional ultrasound system. Besides, elasticity of liver tissues can be shown in both numerical values and color (i.e. higher stiffness is reflected in red color), which can reflect the relative stiffness of the liver tissue quickly. The numerical values can be expressed in either kPa or m/s, which can be comparable with the results from transient elastography or ARFI.[37] Actually, its accuracy is higher compared to transient elastography or AFRI in assessing the degree of fibrosis, especially in those with early-stage liver fibrosis.[38] SWE with spleen stiffness index is recommended as the first line assessment for patients with liver fibrosis due to chronic hepatitis C in the latest guidelines.[39] However, only a few studies validate its clinical application.[38,40]
MRE
MRE adopts a phase contrast imaging method which depends on mechanical wave propagation to assess the degree of liver stiffness.[41] Generally, MRE is less operator-dependent and involved in less technical failure. The global picture of the liver can be viewed easily, regardless the obesity or severity of the ascites of the patients. It can also give a comprehensive assessment for the associated complications, for example portal hypertension or associated spleen stiffness.[42] Meanwhile, it is useful for diagnosis and staging of liver fibrosis, even if the fibrosis is very mild. Another advantage for MRE is that the results are readily reproducible.[42] However, MRE is more expensive and time-consuming compared to ultrasound-based approach. Respiration creates artifacts on the images. Another important limitation is that it is not applicable on patients with iron overload, or hemochromatosis, because iron might create noise for the signals received by the MR machine.[43] There are still limited studies mentioning the clinical significance of MRE results. Even though it is apparently sensitive to mild liver fibrosis, the result may sometimes be unreliable.[44]
Serum test formulae
Common laboratory parameters
Another commonly adopted non-invasive assessment is based on serum with or without clinical parameters. Examples including common parameters in clinical practice include aspartate aminotransferase (AST) to platelet ratio index (APRI),[45] Forns index,[46] Fibrosis-4 (FIB-4),[47] Fibroindex,[48] Hui index,[49] NAFLD fibrosis score (NFS)[50] and BAAT score[51][Table 1]. These parameters are derived from routine liver biochemistry panel, so it is quite convenient. These parameters are also technically easy to obtain and with minimal inter-observer variations. Patients with advanced fibrosis can be identified by these tests.[52] However, these parameters are often validated in just one or two liver diseases. For example, two scoring systems for CHC patients, namely APRI and FIB-4, are found to be not useful in CHB patients.[53]
FibroTest®
Some specific biochemical parameters related to fibrinolysis or fibrinogenesis are developed to improve the specificity of liver fibrosis assessment [Table 2]. One example is FibroTest® (BioPredictive, Paris, France; or known as Fibrosure® in the United States ) consists of 5 components, namely GGT, total bilirubin, α-2 macroglobulin, apolipoprotein A1, and haptoglobin. Sometimes, another test, ActiTest, would also perform together with FibroTest® for assessment for liver activity, with the additional measurement of ALT. The results would be adjusted according to age and gender.[54] FibroTest® is originally used in patients with CHC.[55] Nowadays it is recommended by different associations concerning liver studies for evaluation of liver fibrosis in patients with CHB, NAFLD or alcoholic liver disease.[56–58] It is highly reliable and applicable,[59] even for patients with obesity.[60] It performs well for diagnosis of liver cirrhosis for disease entities other than CHC. However, the results are suboptimal for detecting earlier stages before cirrhosis.[61]
Table 2
Different non-invasive approach
| Non-invasive tests | Features | Advantages | Disadvantages |
|---|---|---|---|
| Radiological | |||
| Transient elastography | Ultrasound-based liver stiffness measurement by shear wave velocity by a specific probe | Useful across different liver disease entity. Special probes designed for different body built. Measure liver fat at the same time with CAP. Can identify no or minimal fibrosis | Less reliable in obese patients. Less reliable in severe acute exacerbation of hepatitis. Less reliable in post-treatment fibrosis stages in CHB or CHC patients |
| Acoustic radiation force impulse imaging | Ultrasound-based wave propagation speed measurement by conventional probe | No additional apparatus except ultrasound machine. Can reflect disease progression. Real-time results. Less technical difficulties. Accurate in overweight or obese patients | Narrow range of measurement. Difficult to define a cut-off. More experienced operators need |
| Shear wave elastography | Ultrasound measurement of shear wave velocity | No additional apparatus except ultrasound machine. Elasticity can be reflected by numbers or colors. Sensitive for early-stage fibrosis. Results can be expressed into kPa or m/s | Limited studies on its clinical application |
| Magnetic resonance elastography | Phase contrast imaging depending on mechanical wave propagation | Less operator-dependent and less technical failure. Limited effect by obesity or ascites. Can assess complications. Sensitive for early-stage fibrosis. Reproducible results | High cost. Limited availability in some countries/ regions. More time-consuming. Not applicable on patients with iron overload or hemochromatosis. Limited studies on its clinical application |
| Serum test formulae | |||
| Common laboratory parameters | Refer to Table 1 | Results from routine liver function test, convenient to perform. No inter-observer variations | Cannot be used for all chronic liver diseases |
| FibroTest | Consists of GGT, total bilirubin, α-2 macroglobulin, apolipoprotein A1, and haptoglobin | Useful in different chronic liver disease. Reliable. Applicable. Accurate in overweight or obese patients | Suboptimal for early stage fibrosis |
| FibroMeter | First 2 generations: consists of platelets, prothrombin index, AST, α-2 macroglobulin, hyaluronate, urea and age. 3rd generation (3G): hyaluronate does not take into account | With high fibrosis classification accuracy. Good predictive value for severe fibrosis in different liver disease entities | High cost |
| Enhanced liver fibrosis | Consists of 3 direct blood markers: procollagen III amino terminal peptide, hyaluronic acid and tissue inhibitor of metalloproteinase I | Good prognostic factor for clinical outcomes in patients with chronic liver diseases. Similar results by using fresh blood or cryopreserved blood. Sensitive for advanced fibrosis or cirrhosis | Not sensitive for early stages of fibrosis. Age, low CD4+ T-cell count and other factors can affect ELF results |
AST: aspartate aminotransferase; CAP: controlled attenuation parameter; CHB: chronic hepatitis B; CHC: chronic hepatitis C; ELF: enhanced liver fibrosis
Research and Real-World Experiences on Cirrhosis Reversal
Firstly I should start out by stating that previous to the introduction of Hepatitis C treatment with DAAs the general position of the medical world was that liver cirrhosis was irreversible. Indeed many medical practitioners still believe this to be true, particularly those who did their training in the 20th century and have not kept up to date with the latest research on liver cirrhosis.
Anti-inflammatories
An important part of reversing liver cirrhosis is reducing or removing inflamed liver cells. The simplest way that this can be approached with known natural anti-inflammatories such as turmeric. Reducing inflammatory cells in the liver
For this, healthy hepatocytes and non-parenchymal cells change the microenvironment from a pro-inflammatory ambience (environment) to resolution, so that the presence of anti-inflammatory mediators increases. The liver macrophages become a restorative phenotype, increasing the expression of MMP and growth factors leading to hepatocyte recovery.
Macrophages, which are key cellular components of the liver, have emerged as essential players in the maintenance of hepatic homeostasis and in injury and repair processes in acute and chronic liver diseases. Upon liver injury, resident Kupffer cells (KCs) sense disturbances in homeostasis, interact with hepatic cell populations and release chemokines to recruit circulating leukocytes, including monocytes, which subsequently differentiate into monocyte-derived macrophages (MoMϕs) in the liver. Both KCs and MoMϕs contribute to both the progression and resolution of tissue inflammation and injury in various liver diseases. The diversity of hepatic macrophage subsets and their plasticity explain their different functional responses in distinct liver diseases. In this review, we highlight novel findings regarding the origins and functions of hepatic macrophages and discuss the potential of targeting macrophages as a therapeutic strategy for liver disease.
The liver is one of the only organs in the body that is able to replace damaged tissue with new cells rather than scar tissue. For example, an overdose of acetaminophen (Tylenol) can destroy half of a person’s liver cells in less than a week. Barring complications, the liver can repair itself completely and, within a month, the patient will show no signs of damage.
However, sometimes the liver gets overwhelmed and can’t repair itself completely, especially if it’s still under attack from a virus, drug, or alcohol. Scar tissue develops, which becomes difficult to reverse, and can lead to cirrhosis
Liver fibrosis
For the 52 patients with nondetectable HCV-RNA with standard methods, the biochemical tests (at a group level) indicated a statistically significant improvement (Table 2). The number of patients with fibrosis score F0–F1 increased from 19 before treatment to 41 at long-term FU. Comparisons were not possible in seven patients because of missing biopsy data at baseline (n=4) or missing TE/biopsy at FU (n=3; Table 2). Overall, the assessed fibrosis stages were significantly lower at FU (P=0.001; Fig. 2).
- Post Categories
- Uncategorized
Greg Jefferys
1 Comment
Leave a Comment Cancel Reply
Join my Hep C Support Group.
Talk privately to other people
with Hep C in a closed group.
Disclaimer
Greg Jefferys’ blog is provided for informational purposes and is not intended as Medical advice, diagnosis, or treatment.
Whilst Greg Jefferys is doing a PhD it is not in medicine. Any advice offered is offered in good faith and based on an extensive general knowledge of Hepatitis C and access to generic Hepatitis medicines Greg Jefferys has acquired through his work as an advocate and activist
The Hep C Buyers Club is not a company or corporate entity but simply a loose structure intended to offer a free information to people with Hepatitis C
Other Books
Click here for other books by Greg Jefferys.
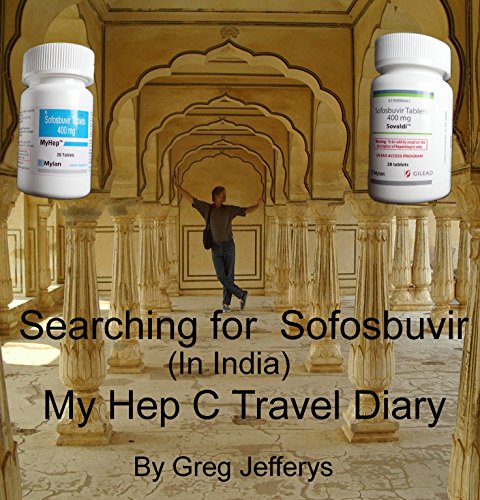
for Kindle
I have converted this diary into a kindle book for folk who might like it in that format. I have added a lot more depth than the original diary contains, it’s more of a complete story in book format. I have priced it as low as Kindle allows me to @ 99 cents. If you are interested just click here to go to the Kindle page.
Recent Posts
-
Hepatitis C Treatment and Liver Cancer June 19, 2024
-
Motivate C a Profitable Hep C Initiative April 29, 2024
-
After Hep C Healthy Liver Diet September 4, 2023
-
Fear of Hep C Treatment April 14, 2023
-
My Letter to Joe Biden March 2, 2023
-
Dormant Hepatitis C November 27, 2022
-
How Much water to drink during Hep C treatment October 13, 2022
-
Hep C and Peripheral Neuropathy August 21, 2022
-
Fatigue Brain Fog and Hepatitis C August 18, 2022
-
Hep C and Liver Cancer May 18, 2022
Contact Us
If you have any questions please reach out by email, or complete the below form.
Greg Jefferys3439 Channel Highway, Woodbridge, Tasmania, 7161.
Email: gregjefferys@outlook.com


Very interesting, and good to know that our beautiful liver can heal from scarring and cirrhosis.
thank you for this information.